UPDATED NOVEMBER 2023
Jump to a section:
- General Questions
- Agriculture Related Questions
- Long COVID
- Vaccines
- Testing
- Treatment
- Face Coverings
The guidance shared here is from a team of public health professionals at UMASH and is not medical advice. If you can, talk to a healthcare practitioner to learn more and get specific recommendations for you and your health.
When inside, especially in poorly ventilated areas, respiratory droplets stay in the air and flow throughout the same space longer, meaning you’re more likely to breathe in the droplets at a rate high enough to get COVID-19. This is why good ventilation, like opening windows, having portable air purifiers, and HVAC filters, are important indoors.
- Stay up to date with COVID-19 vaccines.
- Improve ventilation while indoors.
- Get tested for COVID-19 if you have symptoms.
- Stay home if you have COVID-19.
- Avoid contact with people who have COVID-19.
- Wear a respirator if you are taking care of someone with COVID-19 to keep yourself safe.
Read more about these recommendations from the Center for Disease Control and Prevention.
 Corsi-Rosenthal boxes:
Corsi-Rosenthal boxes:
Corsi-Rosenthal boxes are easy and inexpensive DIY air cleaners you can make using a fan and air filters. These boxes significantly reduce viruses in the air, and can also reduce the levels of other harmful airborne particles. Faculty, students and staff in the Division of Environmental Health Sciences at the University of Minnesota School of Public Health (SPH), including several members of UMASH, recently constructed several of these boxes. Read more in the SPH story.
For some farmers, it is difficult to take days off when operating a farm. This is especially true on farms with daily tasks, like feeding or milking livestock, that need to get done. In this situation, the decision to do farmwork will likely depend on how sick you are, your overall health, and the type of jobs you are doing. If you have to come into close contact with others during your work, it is important to stay home or wear a respirator the entire time.
Looking for a place to find connection? Keep an eye out for upcoming Cultivating Resiliency events. For additional resources, check out the UMASH Stress and Mental Health page to learn about the signs and symptoms of stress and find national and local resources that can support you.
The good news is most people do recover from Long COVID. Getting vaccinated can make it less likely that you will experience Long COVID since those who are vaccinated often do not get as sick from the virus. If you think you might have Long COVID, it is best to see a healthcare practitioner to find out the cause of your symptoms and understand your treatment options.
Some people, especially those with low income or without health insurance, may hesitate to see a healthcare practitioner because they are worried about how they will be able to pay for the appointment. To help reduce this barrier, the Health Resources and Services Administration (HRSA) has created a tool called “Find a Health Center” that can help you locate low to no-cost healthcare.
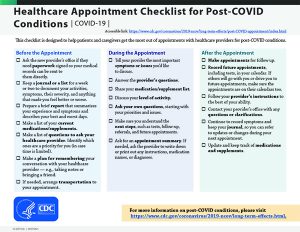
If you think you may have Long COVID and are able to see a healthcare practitioner, prepare for your appointment by using these tips, including keeping a list of your symptoms in the weeks leading up to the appointment and preparing questions to ask your practitioner about your symptoms, treatment options, and more.
Health Equity
It is important to recognize that some people who seek out healthcare for their symptoms of Long COVID may not feel like their healthcare practitioner listens to or believes their health concerns. Some patients may experience stereotyping, discrimination, or assumptions based on their race, gender, body size, disabilities, existing health conditions, and more. People with multiple marginalized identities, like Black women with disabilities, continue to experience some of the most intense medical discrimination. Although there is not an easy fix to this problem, an organization called Patients Rising provides a helpline and website resources to help patients become stronger advocates for their health. If you are interested to read about how many professionals and researchers are working to improve health and well-being for everyone, check out the healthcare research from the Research Library at the Center for Antiracism Research for Health Equity.
Currently, there is not a single treatment for Long COVID. Most of the treatments currently available are to help manage the symptoms of Long COVID. Sometimes, a combination of treatments is needed to improve symptoms. Some examples of treatment options could include physical therapy and rehabilitation for physical symptoms, medication, counseling, and other support. If you think you may have Long COVID, we encourage you to see a healthcare practitioner if you can.
To learn more about how the COVID-19 vaccine works, what to expect, and more, check out the Minnesota Department of Health’s COVID-19 Vaccine Basics Factsheets available in English, Spanish, Hmong, and Somali.
- COVID-19 Vaccine Basics (English)
- Koob Tshuaj COVID-19 Qhov Tseeb (Hmong)
- Xogta Aasaasiga eh ee Tallaalka COVID-19 (Somali)
- COVID-19 Puntos Básicos (Spanish)
The original COVID-19 vaccine, released in 2021, was a monovalent COVID-19 vaccine. This vaccine strengthened the immune system against the original strain of the COVID-19 virus. The 2022-2023 bivalent vaccines were designed to protect against both the original strain of COVID-19 and the previous Omicron strains that were spreading. These vaccines are no longer available because the 2023-2024 updated COVID-19 vaccine was released, giving you better protection against COVID-19.
Getting the most updated COVID-19 vaccine gives you the most protection against the current strains of the virus.
Wondering if you are up to date with your COVID-19 vaccines? Check out the CDC’s vaccine recommendations. This page updates regularly to provide you with the most current vaccine information.
If you have recovered from COVID-19, some people choose to get vaccinated right away, especially if they live in an area where COVID-19 hospitalizations are high, are personally more likely or around others who could get really sick if they got COVID-19.
However, if you have multisystem inflammatory syndrome, you should wait 90 days before receiving your updated COVID-19 vaccine. The CDC has also said that people “may consider delaying your next vaccine by three months” after having COVID.
We know these recommendations are a bit confusing and always changing. Talk with your healthcare practitioner to find out what vaccine timeline they recommend for you after having COVID-19.
- Children who are less than 6 months old are currently not eligible to get the 2023-24 COVID-19 vaccine. .
- Children between the ages of 6 months to 5 years who have received a previous COVID-19 vaccine may need one or two of the 2023-2024 updated COVID-19 vaccines to be up-to-date.
- Children between the ages of 6 months to 5 years who did not receive any of the previous COVID-19 vaccines are unvaccinated and may need two or three of the 2023-2024 updated COVID-19 vaccines to be up-to-date.
- People with certain health conditions may have a unique vaccine schedule tailored to their individual health by their healthcare practitioner.
All of these exceptions can be confusing. Talk to a healthcare practitioner to find out how many vaccines you need to be up-to-date. Keep in mind, these recommendations change often so check the CDC for the most updated vaccine recommendations.
Most people with Medicare, Medicaid or private health insurance are able to get a COVID-19 vaccine for free. People who do not have insurance or whose insurance does not cover their vaccine can get free vaccines through the CDC’s Bridge Access Program. To find places to get your vaccine that are part of this program, enter your zip code in the Vaccine Locator and look for vaccine locations that are listed as a “Bridge Access Program Participant”.
- If you have symptoms, get tested immediately.
- If you were exposed to someone with COVID-19 but do not have symptoms yourself, wait five days to get tested.
- Get tested when you are required to do so, like for travel, your job, or certain events.
- Consider getting tested if you plan to be around someone with a weakened immune system or is more likely to get really sick from the virus.
To learn more or read about the most current testing guidelines, visit the CDC’s COVID-19 Testing page.
Antigen tests can be easier and faster to get since you can buy a test yourself and get results within minutes. However, the downside of antigen tests is that they can be less sensitive in detecting if you have COVID-19, especially early on in the infection. This means that there is a chance that the antigen test may tell you that you don’t have COVID-19 when you actually do have the virus. However, when the test does give a positive test result, it is usually correct. This means that if the test tells you that you have COVID-19, you can feel very confident that you actually do have the virus.
You can also buy antigen tests at most pharmacies. Some insurances may cover COVID-19 tests. Call your insurance company or ask your pharmacist to find out if they are covered under your insurance.
FREE AT HOME TEST KITS AVAILABLE IN MINNESOTA AND IOWA:
Rather get tested in person? You can find your closest testing site using the Center for Disease Control’s Testing Locator.
A second treatment option, called convalescent plasma, is available for some people with weakened immune systems. For this treatment, a person with COVID-19 gets an IV infusion of plasma from someone who has recovered from COVID-19. This treatment can help their immune system fight the virus.
Most of these treatments need to be started within the first few days of having symptoms, so talk to your healthcare practitioner right away to see if any of these treatment options are right for you.
If you are positive for COVID-19 and want to get treatment, you have a few options to access treatment:
- Contact your healthcare practitioner and request treatment. This practitioner can help you weigh the risk and benefits of getting treatment. If you decide to get treatment, they can help identify which treatment is best for you.
- Find a pharmacy or clinic that offers treatment. You can use the COVID-19 Test to Treat Locator through the Administration for Preparedness & Response to find locations that can test you for COVID-19, offer treatment, and fill prescriptions. This tool also shows you which treatment options are available at each location.
- If you live in Wisconsin or Minnesota, you may be able to get prescribed antiviral treatment for COVID-19 through a telehealth appointment at no cost. The Wisconsin COVID-19 treatment program will be offered to Wisconsin residents at least through December of 2023.
Experts at the Center for Infectious Disease Research and Policy have strongly recommended wearing a respirator (like an N95 or KN95) instead of a cloth or surgical mask. Cloth and surgical masks do not offer enough protection against the virus. As experts have learned more about COVID-19, they have found that the particles of COVID-19 that travel through the air and cause the virus to spread are very, very small. These small particles pass easily through cloth and surgical masks. Respirators do a much better job at preventing COVID-19 particles from entering your mouth or nose.
- If you live in an area where COVID-19 is rapidly spreading. Enter your zip code in the CDC’s COVID-19 County Check tool to see what COVID-19 is like in your county.
- If you are positive for COVID-19 and are unable to isolate yourself in a separate room from others. This will make it less likely that you will spread the virus to other people around you.
- If you are caring for someone with COVID-19. COVID-19 can spread easily between people, so it is important to wear a mask to protect yourself.
Don’t forget! You should still wear NIOSH-approved respirators when farm tasks expose you to grain dust, pesticides, toxic chemicals or infectious diseases.
- Looking for guidance for choosing a type of respirator for your specific farm task? Check out the Agricultural Respirator Selection Guide from AgriSafe.





 Download testing recommendation fact sheets from the Minnesota Department of Health:
Download testing recommendation fact sheets from the Minnesota Department of Health: I have more questions. Where can I find more information?
I have more questions. Where can I find more information?